You can also check out this episode on Spotify!
Three years after the World Health Organization declared the COVID-19 pandemic, we have widespread population immunity against the virus. But no one is immune to accumulated fear and uncertainty.
On this episode, Dr. McBride talks about where we are now and what to expect with COVID. She discusses various topics including
the transition from pandemic to endemic
rapid antigen versus PCR testing
treatments, including Paxlovid
the recent Cochrane review on masks and mask mandates
vaccines and immunity
what to expect in fall 2023
addressing our pandemic story
Finally, Dr. McBride argues that recovering from the distress of last three years requires understanding our unique risks and risk tolerance—and appropriately reckoning with vulnerability.
Join Dr. McBride every Monday for a new episode of Beyond the Prescription. You can subscribe on Apple Podcasts, Spotify, or at lucymcbride.com/podcast.
Get full access to her free weekly Are You Okay? newsletter at https://lucymcbride.substack.com/welcome
Please be sure to like, rate, review — and enjoy — the show!
The full transcript of the show is here!
Hello, and welcome to my home office. I'm Dr. Lucy McBride, and this is "Beyond the Prescription." Today, it's just you and me. Every other week this season, I'll talk to you like I do my patients, pulling the curtain back on what it means to be healthy, peeling back the layers of everyday medical problems I see. In clinical practice for over 20 years, I've found that patients generally want the same things, a framework to evaluate their risks, [00:00:30] access to the truth and the courage to face it, and tools and actionable information to be healthy, mentally and physically. So, whether it's managing weight, cholesterol, cancer, or mental health issues, we all want to feel more in control of our health. Here, I'll talk to you about how to be a little more okay tomorrow than you are today, and how to be healthy from the inside out. Let's go.
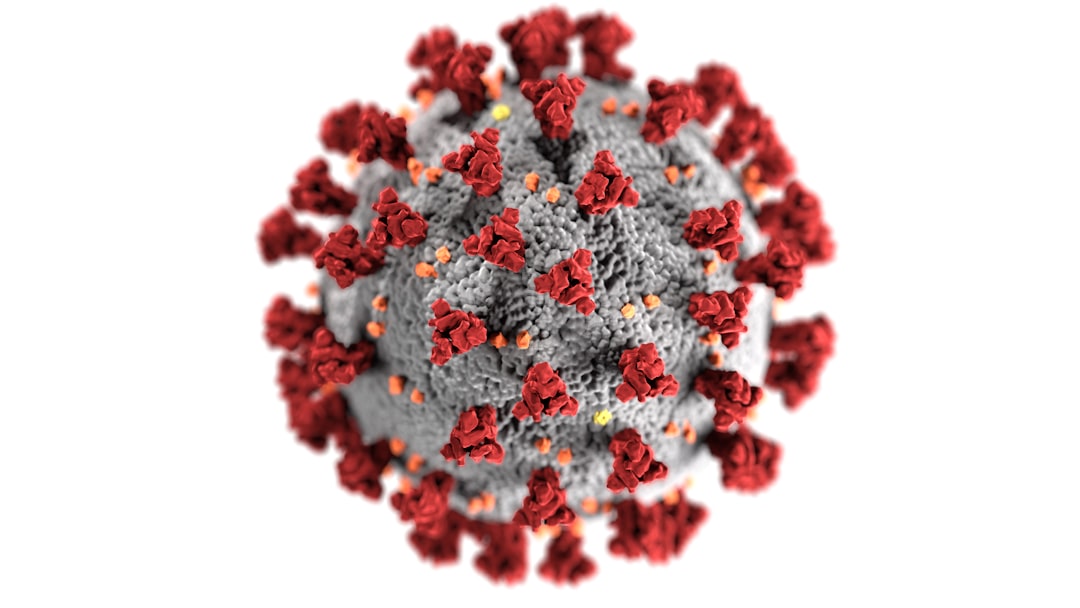
Today is a little ditty about COVID-19, my friend and foe for the past three years. Something you have probably thought quite a lot about, that has probably occupied a fair amount of real estate in your brain and in your everyday life for the past three years. Let's talk today about where we are now, where we have been, and where we're going with this virus. It's the three-year anniversary of the World Health Organization's declaration of the pandemic. That was on March 11th, 2020, and over the last three years, we have learned so much. We have [00:01:30] learned about the virus, about immunity; we've learned about how to protect the most vulnerable among us.
We've also learned about ourselves. We've all had to reckon with grief, loss, uncertainty, and significant vulnerability. So, let's take a minute to talk about COVID itself. We'll talk about symptoms, testing, isolation, the vaccines, boosters, and where we might go from here. Okay. So, first of all, [00:02:00] let's acknowledge, COVID is here in perpetuity. It has now been woven into the fabric of our everyday lives, whether we like it or not. It is endemic. Endemic means hospitals are no longer overwhelmed from COVID-19. It means that the vast majority of people in this country and around the world have some sort of immunity to the virus, either from the vaccine or from past infection, and that we have widely-available vaccines and therapeutics. Endemic does not mean that we are done with COVID-19. [00:02:30] No, no. COVID and COVID risk are something we will have to reckon with here on out.
What's happening with the virus right now? Well, the virus is here. In D.C., I'm seeing a couple patients a week with COVID-19. They mostly have typical cold or flu symptoms and are doing generally very well with at-home remedies like Tylenol, Advil, hydration, and rest. Now, some of my patients have been sicker, like patients who are older, who have underlying health conditions, like lung disease, for example. But it's important to note [00:03:00] that they're as sick as they probably would have been with another respiratory virus—one that we have known about since pre-pandemic times. For example, flu, RSV, metapneumovirus, parainfluenza virus. In other words, we have seen these kinds of respiratory viruses since the beginning of time, and COVID, in the vaccine era, has been added to the list of viruses that we will now be susceptible to, and for whom it is particularly potentially dangerous for people who are at higher risk in general.
What about Paxlovid? [00:03:30] So, Paxlovid is the oral antiviral medication that is FDA-approved, and appropriate for patients who are at particularly high risk for serious COVID outcomes. Who do I prescribe it to in the spring of 2023? The truth is, not many people, because at this point in the pandemic, most people have had COVID-19. Most patients, at least my patients, have had the vaccine, and that protection, that hybrid immunity, the combination of vaccine-induced and infection-acquired immunity, is marvelously protective against serious COVID outcomes, such that Paxlovid is not really necessary. Paxlovid has some downsides as well. So, when the upsides are minimal, and the downsides are not zero, it's worth a conversation to explain, not to hang our hat on Paxlovid as a panacea, and more importantly, to have confidence in our own immune system, and the marvelously effective vaccines, to protect us when we need it. Do I still prescribe Paxlovid? Absolutely. It's just a nuanced discussion, and one that the headlines really can't capture.
So, what about booster shots? Are we going to need a booster [00:04:30] shot every fall, like we need the flu shot? Well, the short answer is we don't know. Right now, public health agencies are predicting that they'll roll out an annual COVID shot like we do the flu shot. And this fall, when we're indoors, in crowded, poorly-ventilated spaces, we might need a booster shot. But that's not based on any particular science. It's based on the emerging evidence that there's a seasonal component to COVID, like there is for so many respiratory viruses. What that projection is not based on is the clear evidence that everyone will absolutely need a booster in the fall. That would not be accurate to project. In fact, right now, in 2023, immunity from the vaccine and from past infection continue to do a marvelous job at protecting us where it counts, preventing severe disease, and mitigating but not blocking transmission.
Remember that the vaccine can no longer protect against infection. The current variants, which are Omicron sub-sub-variants, are so highly contagious [00:05:30] that they outskirt the antibodies made by vaccination and from past infection. What that means is that you can get 3, 4, 5, 10 vaccine doses with the current vaccine formulation and still get COVID-19. You're just very unlikely to land in the hospital, and your symptoms will be mitigated if you've had a recent vaccine or recent bout of COVID itself. So, when people talk about waning immunity, that refers only to the antibody levels that inevitably and normally fall over time, three to four months after a shot or after an infection. If our antibody levels did not wane after exposure to a vaccine dose or a virus, our blood would be a thick milkshake full of antibodies. So indeed, those antibody levels go down with time, but our immunity against serious outcomes is lasting. How long will it last? We don't know. But at least for right now, people who have had vaccine doses for their age and underlying health conditions, [00:06:30] and/or who've had COVID itself, are not landing in the hospital from COVID-19 more than they would have from other viruses at this moment.
Are people still being hospitalized for COVID and people dying from COVID-19? They are. And these are people who are our most high-risk patients. They are also patients in the hospital who have so many underlying health conditions that COVID tips them over the edge. This has been true since the beginning of time, that viral infections often tip the balance [00:07:00] in an otherwise very fragile patient. This is not to dismiss the loss and ongoing deaths from COVID-19. It's to frame it in the context of other respiratory viruses, so that you can better understand where we are now and where we might be going.
What about long COVID? Well, the latest data are very reassuring. It looks like the tail of symptoms from COVID-19 are not a whole lot different from other respiratory viruses. Fatigue, difficulty mounting the appropriate blood pressure response when going from lying to sitting to standing, [00:07:30] tachycardia, exercise intolerance, all of these symptoms can be indeed very debilitating, but it turns out the typical symptoms of long COVID are akin to symptoms of the long tail from other viruses.
Are there exceptions? Absolutely. Are some people uniquely susceptible to COVID-19? Yes. Is COVID-19 a virus that can turn on genes that were latent? Absolutely. I talked to a patient today whose child developed type 1 diabetes one [00:08:00] month after recovering from COVID-19. They have no family history of diabetes. What seems clear is that the child developed diabetes as a direct result of the virus. It has long been known that viruses can turn on latent genes, and COVID-19 is no exception. It can turn on autoimmunity. It can tickle someone who has a genetic predisposition to, for example, rheumatoid arthritis. It can mess with our immune system in unusual ways. But the majority of people with COVID-19 make a full recovery, and the tail of symptoms go away with time. There's some interesting emerging evidence that a medication called metformin, which is one of the standards of care for type 2 diabetes, can help with the inflammation of long COVID. There's also some interesting data in the pipeline about Paxlovid, and other protease inhibitors like Paxlovid, that may help with the long tail of COVID-19 symptoms, that might help mitigate the long tail of COVID-19 symptoms.
Let's talk about how to protect ourselves from COVID-19 here on out. [00:09:00] Let's start with my favorite/not so favorite subject, masking. Masking has become the most incredible political football I've ever seen. I have gotten myself so entangled in the mask debate that I almost can't talk about it, but I need to, and I want to. Data from the Cochrane Review on masking came out a couple weeks ago. The Cochrane Review is a systematic review and meta-analysis of the evidence on any specific topic, like masking, and it's really considered [00:09:30] the gold standard in evidence-based medicine. So, when the Cochrane Review comes out with a statement, people tend to listen. Here's what they said about masks. "Mask mandates failed to reduce transmission of COVID-19 during the pandemic."
I'm just gonna repeat that, for people on the back. Mask mandates have not been shown to reduce the transmission of COVID-19. Let's break that down. Does this mean that masks do not work? It does not. [00:10:00] It means that the public policies that asked people to wear masks in schools and workplaces, on public transportation, did nothing to halt the transmission of COVID-19. Why that is, we could talk about all day long, but the fact of the matter is that mandates have had no meaningful effect, and I will say, because I just can't help myself, that this data has been around since at least 2021. Deep breath. Exhale. So, does this mean that masks [00:10:30] don't work on individuals? It does not. Masks certainly can work on individuals to protect the wearer, but only if the mask is high-grade, well-fitted, and worn consistently. Should you wear a mask in your public transportation, in your conference, at your workplace? At this point, it's really up to you. There's no role for mandates, in my opinion, given the absence of data to show that they worked, and given that this virus is here in perpetuity, and, in my humble opinion, there was [00:11:00] never a role for mask mandates. What I do think is that people should be given the facts and the information about how effective masks can be for the wearer if and when they use them appropriately.
I recommend wearing a mask, if you want to, to help reduce the likelihood of getting infected with COVID-19, with the understanding that they aren't that effective. They can help. They are another layer. The setting in which I would definitely wear a mask to protect myself against COVID-19 is, for example, in an ICU room that is teeming with virus, in which I was the medical provider, I would wear a fit-tested N95 mask in that room. But in 2023, with most of us having immunity from the vaccine and from past infection, a mask that is sort of loosely around your face, that you take on and off for eating and drinking, on the airplane or at the restaurant, is really wearing us for protection at this point. I don't shame anyone for wearing a mask. It is up to their unique risk tolerance, [00:12:00] and it is certainly an added layer, albeit weak, to help mitigate the risk. Better than any mask, however, to protect us from getting infected with COVID, or reinfected, is to open doors, open windows, and avoid crowded, indoor, poorly-ventilated spaces.
And then I think it's important to zoom out on the conversation about risk. There is a risk of getting COVID-19 wherever we go now, certainly more indoors, and more in crowded spaces. There is also the potential harm of having to live in [00:12:30] fear and to hem in our lives to avoid a respiratory virus against which most of us are already immune. My job as a physician is not to tell people how much risk they want to undertake, how much they should sacrifice to not get a virus. It's my job, rather, to arm people with the facts, tools, and information they need to make appropriate risk decisions based on their preferences, goals, and tolerance for disease.
The principle in public health is called harm reduction. Harm reduction is a principle that acknowledges [00:13:00] that risk is everywhere, that we cannot mitigate risk to zero, and that the goal of medicine and public health is to help people mitigate risk without pretending that we can eliminate it. So, what do you do now if you get COVID-19? Should you call your doctor? Should you stay at home? How long should you isolate? Do you test? A lot of my patients are not even calling me and telling me they have COVID. They will tell me at their annual physical, oh yeah, I had COVID a month ago, I tested positive on the rapid test, I stayed at home until I felt better, and then I went back to work. [00:13:30]
The rapid tests continue to be an excellent tool. The rapid tests are contagiousness tests. The rapid tests tell you when you have high enough levels of virus in your nose to A, make a diagnosis of COVID, but more importantly, they tell you that you're contagious. When a rapid test is positive, it means you're contagious to other people. When the rapid test is negative, it means you're no longer contagious. The rapid tests tell you when you have enough virus in your nose to infect someone else. How long those COVID-19 rapid home [00:14:00] tests are positive after you have symptoms or test positive is so variable. Some people test positive for one day. Some people test positive for 10 days. What the rapid antigen tests cannot do is they cannot tell you the degree of contagiousness. They can't tell you what is probably true, which is that 10 days out, you're probably less contagious than you are at 3 days, even if you're positive on both of those days. When you should go back to work is really up to you and your risk tolerance. Most likely, just like with [00:14:30] other viruses, when you've been fever-free for 24 hours, your symptoms are improving, and you've got your normal energy back, you're probably not that contagious. But still, the rapid antigen tests are considered contagiousness tests.
What about a PCR test? So, the PCR test, remember, the PCR tests are still the gold standard for diagnosis. In other words, if someone has a stuffy nose, sore throat, and congestion, and they're negative on a rapid test, that means that they're not contagious with COVID-19. It doesn't mean they don't have COVID. So, some of those patients, I'll bring in and do a PCR [00:15:00] test for a flu, COVID, RSV, and that will tell us, with good certainty, whether or not they have those three viruses. For many of my patients recently, they're negative on the home test and positive on the PCR. Why? Because the PCR is extremely sensitive, and the rapid test being negative simply means they're not contagious in that moment. How do you distinguish between spring allergies, flu, RSV, COVID, and all the other things? The answer is testing. A rapid home antigen test, again, means you're not contagious with COVID, but it doesn't mean you don't have COVID. So if you're wondering, go get a PCR test with your doctor.
You can also do a really simple thing which is, if you typically get allergy symptoms this time of year, you might want to get back on your allergy medications, like Allegra and Flonase, and see if your symptoms abate, and if they do, you probably have your diagnosis. If you have any questions about your symptoms, you should see your personal physician.
Here's my final note about COVID-19. I think it's very important to acknowledge to ourselves that we have all experienced some sort of loss. Whether you lost your fourth-grade classroom experience for two years, your high school prom in 2020 and 2021, or you lost a loved one to COVID-19 and you were separated from them in their final hours, whatever your pandemic story is, it's essential to recognize that that story lives in our body, that the emotional, physical, and mental health toll of living through a pandemic is real. And not all of that [00:16:30] suffering is measurable. There's no PCR test for despair. There's no way to quantify the lost opportunities, the absence of social connection, and the isolation that we have experienced during the pandemic, particularly for young people, and for elderly loved ones in nursing homes and assisted living. And then for people with preexisting mental health issues, I think the pandemic has been uniquely traumatizing. I see it in my office. I see the accumulated [00:17:00] stacks, stressors adding up in people's blood pressures, in people's laboratory results, and I see it in their eyes. This is not to say that we are broken. This is not to say we are beyond repair. It is simply to say that health is about more than the absence of COVID-19.
We are the integrated sum of complex parts. Health is about having awareness about the stories we tell ourselves, acceptance over the things we cannot control, and having more agency over our life. [00:17:30] This begins, in my opinion, with having access to fact-based information to care for our body and mind. It's my hope that the reckoning that we've all had to do with our health and well-being during the pandemic helps us zoom out on what it means to be healthy. That definition will be unique for each of us. So ask yourself, what does it mean to you to be healthy? For some people, that means having a perfect cholesterol score. For some people, it means re-engaging in intimate relationships. For other [00:18:00] people, it means taking risks, challenging their vulnerabilities and fears, stepping outside of their comfort zone, challenging their risk tolerance or venturing out beyond their comfort zone. And for all of us, I think it means re-engaging in healthy, strong relationships, taking care of our bodies, prioritizing sleep, and assessing our mental health like we do any other organ system, taking stock of our fears, anxieties, moods, relationships with food, [00:18:30] alcohol, work, and each other. No one is okay on the heels of the pandemic. The question isn't, can you win your annual checkup with your doctor? The question is, how can you be a little more okay tomorrow than you are today?
Thank you so much for joining me. I'll see you next time. Oh, and before I forget, please leave me a comment. I'd love to hear your thoughts, ideas, and definitions of health. Drop me a line below.













Share this post