6 Myths About Menopause That Prevent Women From Getting Appropriate Care
HRT after age 60? Blood testing for perimenopause? Let’s get women the data they need!
ICYMI 👉
6 Reasons Your Sex Life Might Be Suffering—And What to Do About It
A Surprising Fix for Weight Gain, Digestive Woes & Skeletal Pain
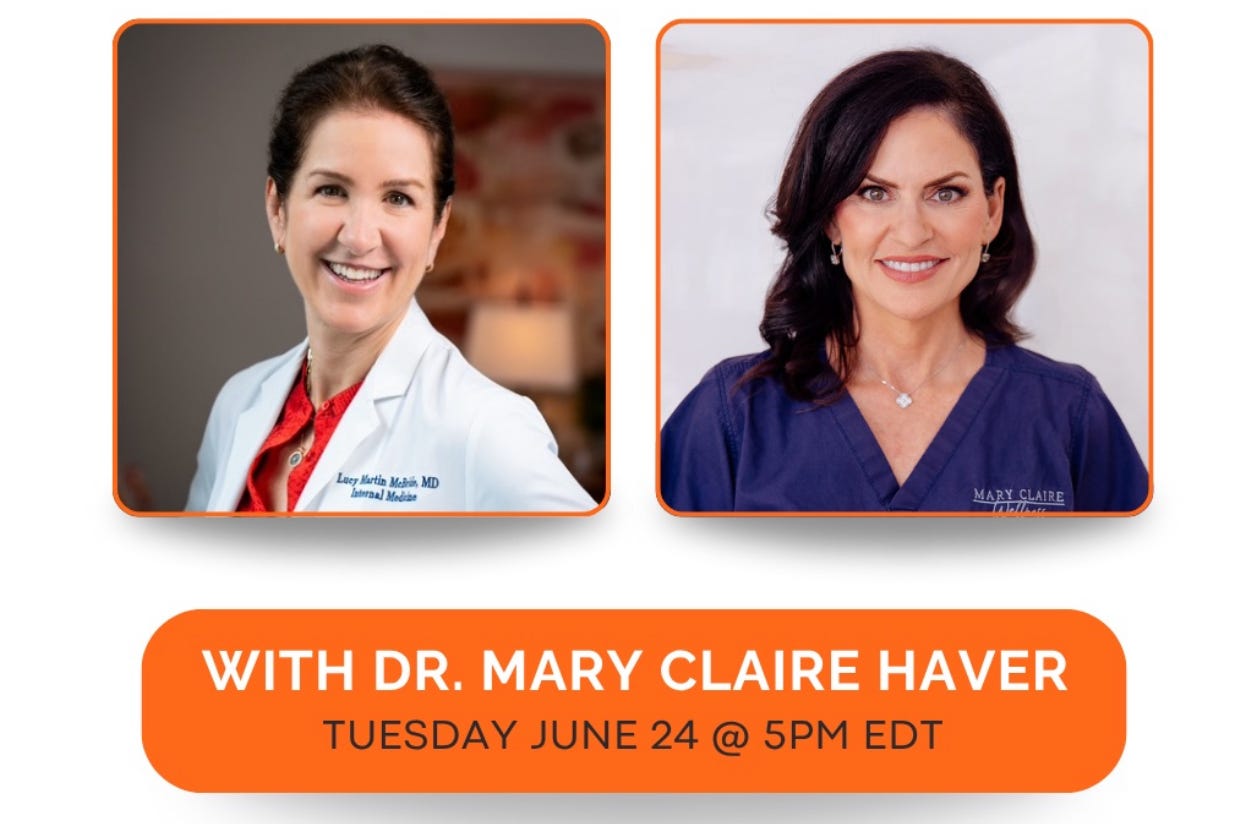
🙋🏻♀️ Join me LIVE at 5 pm ET today—right here! I’ll be talking with the MENOPAUSE QUEEN,
. Dr. Haver is a board-certified OBGYN and author of the NYT bestselling book, The New Menopause. We will discuss the nuances of hormonal health, perimenopause and menopause. Bring your questions!When Sarah came to see me at 47, she was convinced something was seriously wrong. Her periods had become erratic, she was waking up in the night drenched in sweat, and she described her brain as feeling "wrapped in cotton." But when she asked her gynecologist about perimenopause, she was told she was too young and needed to get her hormones tested first to "prove" she was in the transition.
Wrong 🚫
Sarah needed hormone therapy—either the birth control pill or low dose HRT—to ease her transition to menopause.
Then there is my 70 year old patient Ellen whose frequent urinary tract infections (UTIs) and hip pain caused her to bounce around from one specialist to the next. Her orthopedist insisted it was arthritis causing her pain. Her urologist counseled her to prevent UTIs by drinking more water and urinating after sex. When Ellen asked about HRT for vaginal dryness, her urologist told her it was out of the question because of her family history of breast cancer.
Wrong 🚫
A family history of breast cancer isn’t a contraindication to HRT. Moreover, Ellen’s symptoms had everything to do with estrogen depletion (i.e., menopause). She needed two things to feel back to herself: 1) vaginal estrogen therapy to treat the genitourinary syndrome of menopause and 2) pelvic floor physical therapy to stabilize her hip joint from the inside out.
Both Sarah and Ellen had been caught in a web of common misconceptions about menopause that delay diagnosis and proper treatment for millions of women every year.
The misinformation surrounding menopause isn't just frustrating—it's actively harmful. These myths keep women suffering unnecessarily, prevent them from accessing effective treatments, and perpetuate the medical dismissal that has characterized women's healthcare for far too long.
Let's examine six persistent myths about menopause that you need to stop believing if you want to become an effective advocate for your own care.
Myth #1: You Need Hormone Testing to Diagnose Perimenopause & Menopause
This might be the most pervasive myth in menopause care. When women suspect they're entering perimenopause, both they and their doctors often reach for hormone tests, assuming these will provide definitive answers about what's happening.
The reality is that perimenopause is primarily a clinical diagnosis based on your age, menstrual history, and symptom constellation. Checking estrogen, progesterone, and FSH levels during perimenopause can be more misleading than helpful. During the perimenopausal transition, these hormones fluctuate—sometimes from hour to hour within the same day. A blood test captures only a single moment in time, which may have no relationship to how you felt that morning, how you'll feel that evening, or your overall symptom pattern.
You could have a "normal" estrogen level at 9 AM while experiencing debilitating brain fog by 2 PM as your hormone levels drop. Conversely, you might have abnormal hormone values on paper while feeling completely fine. I've seen women with textbook perimenopausal hormone patterns who have no symptoms, and women with "normal" labs who experience debilitating hot flashes and insomnia.
Hormone testing may be useful in specific circumstances, such as evaluating women under 40 with suspected premature menopause, unclear cases where other conditions need to be ruled out, or monitoring response to hormone therapy. But for most women experiencing typical perimenopausal symptoms in their 40s and early 50s, the clinical picture provides more reliable diagnostic information than laboratory values.
The truth: If you're in your 40s or early 50s and experiencing classic perimenopausal symptoms, a blood test isn’t necessary to confirm what your body is already telling you.
Myth #2: Menopause Symptoms Are Mostly About Hot Flashes
While vasomotor symptoms like hot flashes and night sweats do affect about 75% of women, they represent just the tip of the iceberg. The full spectrum of menopausal symptoms is far more complex because estrogen doesn't just regulate reproduction—it's a master coordinator affecting virtually every system in your body. Brain fog and memory issues, sleep disturbances, mood changes, joint stiffness, changes in skin and hair, weight gain around the midsection, decreased libido, and urogenital symptoms like vaginal dryness and recurrent UTIs are all legitimate manifestations of declining estrogen.
This myth is particularly harmful because it leads to underrecognition and undertreatment of the full range of menopausal symptoms. A woman experiencing severe brain fog might be told her "hormones are fine" based on a single lab draw, while her cognitive symptoms continue to impact her work and relationships. Another might endure recurring UTIs treated with multiple rounds of antibiotics because no one connects her symptoms to estrogen deficiency.
Understanding the broad impact of menopause helps explain why effective treatment often addresses multiple symptoms simultaneously. When a patient starts hormone therapy for hot flashes and discovers her joint pain improves and her thinking becomes clearer, that's not a coincidence—it's estrogen's wide-ranging effects being restored.
The truth: Menopause affects virtually every system in your body, and symptoms often appear in unexpected combinations that may not initially seem hormone-related.
Myth #3: Hormone Therapy Is Dangerous for Most Women
This myth has its roots in the 2002 Women's Health Initiative study, which initially appeared to show that hormone replacement therapy significantly increased risks of breast cancer and heart disease. The medical community's response was swift and dramatic: doctors were advised against prescribing HRT except in cases of severely debilitating symptoms, and millions of women were told to "just deal with" their menopausal symptoms.
What happened next represents one of the most significant course corrections in modern medicine. When researchers reanalyzed the WHI data with more sophisticated statistical methods and longer follow-up, they discovered the initial conclusions were overstated and misunderstood. The risks of HRT were highly dependent on factors like age, health status, and timing of therapy initiation.
For the majority of women starting HRT within 10 years of menopause onset (particularly those under 60), the benefits usually outweigh the risks. These benefits include not just symptom relief but also protection against osteoporosis, potential cardiovascular benefits when started early, and possible cognitive protection.
Some factors require careful consideration rather than automatic exclusion from HRT. Family history of breast cancer is not an absolute contraindication. Previous blood clots might favor transdermal over oral estrogen rather than eliminating all hormone options. History of migraines or gallbladder disease requires specialized evaluation but doesn't necessarily preclude hormone therapy.
True contraindications to HRT include active breast cancer, history of endometrial cancer, active liver disease, unexplained vaginal bleeding, and recent history of stroke or heart attack. However, even some of these situations may have exceptions based on individual circumstances and timing.
The key is understanding that both taking and not taking hormones involve risks. Declining estrogen increases risks of osteoporosis, cardiovascular disease, and potentially cognitive decline. The decision should be based on your individual risk profile, symptom severity, and personal values rather than fear-based generalizations.
Current evidence shows that transdermal estrogen (patches or gels) carries lower blood clot risks than oral estrogen, and that bioidentical hormones aren't necessarily safer than conventional formulations. Local estrogen therapy for urogenital symptoms is considered safe for virtually all women, including many with a history of breast cancer.
The tragedy of the post-WHI era isn't just the years of unnecessary suffering—it's that an entire generation of women was denied access to effective treatment based on fear rather than evidence.
The truth: For appropriately selected women, hormone therapy is both safe and effective, particularly when started during the "window of opportunity" early in the menopausal transition.
Myth #4: Natural Remedies Are Always Safer Than Hormones
The appeal of "natural" menopause treatments is understandable, especially given decades of fear-mongering about hormone therapy. Many women turn to herbal supplements, bioidentical hormones from compounding pharmacies, or other alternative approaches believing these are inherently safer than conventional treatments.
This myth is problematic for several reasons. First, "natural" doesn't automatically mean safe or effective. Many plants produce compounds that are biologically active and potentially harmful—poison ivy is natural, but you wouldn't rub it on your skin! Herbal supplements aren't regulated with the same rigor as prescription medications, meaning their purity, potency, and safety aren't guaranteed.
Second, the distinction between "natural" and "synthetic" hormones is often meaningless. Many FDA-approved hormone therapies are bio-identical to human hormones and derived from natural sources. The estrogen in most hormone patches comes from plants, but it's manufactured under strict quality controls that ensure consistent dosing and purity.
Compounded "bioidentical" hormones, despite their natural marketing, often lack the rigorous testing and standardization of FDA-approved products. They may contain varying doses of hormones, and their long-term safety profiles haven't been established through large-scale clinical trials.
This isn't to dismiss all complementary approaches—lifestyle modifications like regular exercise, stress management, and adequate sleep are crucial components of menopause management. Some women find relief with acupuncture or cognitive behavioral therapy. But these approaches work best as part of a comprehensive treatment plan, not as substitutes for evidence-based medical care when symptoms are severe.
The truth: The safety and effectiveness of any treatment depends on the specific substance, its quality, dosing, and your individual health profile—not whether it's labeled "natural" or "synthetic."
Myth #5: You Should Suffer Through Menopause Because It's "Natural"
Perhaps the most insidious myth is the idea that women should endure menopausal symptoms without treatment because menopause is a "natural" life transition. This perspective treats suffering as virtuous and medical intervention as somehow artificial or wrong.
By this logic, we shouldn't treat other natural processes either. Nearsightedness is natural, but we use glasses. Broken bones heal naturally, but we use casts to ensure proper alignment. Pregnancy and childbirth are natural, but we've developed medical interventions that save lives and reduce suffering.
The "natural is better" argument often masks deeper biases about women's pain and experiences. Would we tell someone with diabetes to avoid insulin because elevated blood sugar is their body's "natural" state? Would we suggest that men with erectile dysfunction should accept it as natural aging? The double standard is glaring.
Menopause may be natural, but so is the human capacity to develop treatments that improve quality of life. We have safe, effective therapies for menopausal symptoms backed by decades of research. Choosing not to use them isn't more virtuous—it's just less comfortable.
This myth also ignores the reality that modern lifespans mean women may spend 30-40 years in a postmenopausal state. Our ancestors didn't face this situation because they didn't live as long. We're navigating uncharted territory, and it makes sense to use every tool available to maintain health and wellbeing during these decades.
The truth: Menopause being natural doesn't mean suffering is mandatory or that treatment is unnatural. You deserve to feel well during this transition and beyond.
Myth #6: You Can't Take Hormones After Age 60
This arbitrary age cutoff represents one of the most harmful oversimplifications in menopause care. Many women are told that once they reach 60, hormone therapy is off the table—period. This blanket prohibition ignores individual circumstances, symptom severity, and the significant distinction between different types of hormone therapy.
The 60-year age limit stems from data showing increased cardiovascular risks when systemic hormone therapy is initiated many years after menopause. This "timing hypothesis" suggests there's a "window of opportunity" for safely starting hormones, typically within 10 years of menopause onset or before age 60. But this doesn't mean all hormone therapy becomes dangerous at the stroke of midnight on your 60th birthday.
Most importantly, this myth completely ignores local estrogen therapy, which remains safe and effective regardless of age. Vaginal estrogen—delivered as creams, tablets, or rings—addresses urogenital symptoms with minimal systemic absorption. The amount of estrogen that enters the bloodstream from vaginal applications is negligible, making this treatment appropriate for most women well into their 80s and beyond.
Consider the 72-year-old woman experiencing painful intercourse that's harming her relationship, or the 68-year-old dealing with recurrent UTIs that antibiotics can't fully resolve. These women often benefit dramatically from vaginal estrogen, yet many are told they're "too old" for any hormone therapy. This blanket prohibition condemns women to years of unnecessary suffering from highly treatable conditions.
Even systemic hormone therapy isn't automatically inappropriate after 60. For women with severe ongoing symptoms who started HRT within the appropriate window and have been doing well, continuing therapy may be reasonable with careful monitoring. Some women may benefit from lower doses or different delivery methods. The key is individualized assessment rather than arbitrary age cutoffs.
The evidence also shows that vaginal estrogen is considered safe even for many women with a history of breast cancer, because systemic absorption is so minimal. Yet older women are often denied this treatment based on age alone, regardless of their cancer history or other risk factors.
I spoke about this at length with urologist Dr. Rachel Rubin last week.
The truth: Vaginal estrogen therapy is safe and effective at any age, and systemic hormone decisions should be based on individual risk-benefit analysis, not arbitrary age limits.
Getting the Care You Deserve
Understanding these myths is the first step toward becoming an effective advocate for your menopause care. When you walk into a doctor's office armed with accurate information, you're better positioned to have productive conversations about your symptoms and treatment options.
Prepare for appointments by documenting your symptoms specifically, tracking menstrual changes, and coming with clear questions about your situation. Don't accept dismissive responses like "this is normal aging" without discussion of treatment options. If your provider seems unfamiliar with current menopause guidelines or refuses to consider evidence-based treatments without clear medical reasoning, seek a second opinion.
The North American Menopause Society maintains a directory of healthcare providers who have completed specialized training in menopause management. These clinicians are more likely to be familiar with current research and comfortable prescribing appropriate treatments.
You don't need to be a victim of misinformation or medical dismissal. Armed with facts instead of myths, you can advocate effectively for the care you deserve during this significant life transition. The goal isn't just surviving menopause—it's thriving through it with the support of evidence-based medicine and healthcare providers who listen.
Join me and Dr. Haver today at 5 pm ET!
Link here
Disclaimer: The views expressed here are entirely my own. They are not a substitute for advice from your personal physician.







So glad you are covering this topic with enlightened hope for women suffering in menopause years. And I can personally testify to the benefits of vaginal estrogen cream for so many symptoms, especially for sexual pleasure decades after early menopause with a long perimenopause phase at age 39. I was lucky I had understanding doctors who would prescribe prempro for about seven years and then premarin vaginal cream for decades later even with my breast cancer history. My urologist agrees with me that nothing works as well as estrogen for vaginal dryness and atrophy and UTI prevention.
So - I've survived endometrial cancer and a subsequent spread to my lymph nodes, which I've been in remission from for 6 years. I feel very lucky, but I'm 60, and one of the most persistent issues I've had is fatigue. I just had an echocardiogram, and I'm currently wearing a Zio patch, both in an effort to see if heart function is the source. The echo revealed minor thickening of the left ventricle, but my doctor didn't think it was a problem - just something to be monitored. I've had blood tests, I do have low ferritin, but everything else is "within normal ranges". I'm trying amitriptyline for possible fibromyalgia, but not really noticing anything different. I've also been tested over the years for adrenals/endocrinology but according to the doctors not a source of fatigue. Another issue I've been battling is trying to lose and keep weight off. I did well with the help of weight loss drugs - losing almost 80 lbs, but my insurance quit covering it and I've had trouble sorting out access ever since. Now, after all that, the aggravating part is that none of my doctors can/will dig any deeper. Other things I do include using cpap, which apparently I'm compliant with, and using supplements like melatonin both for sleep and as a cancer preventative, if that is even possible. Sorry for the huge post -but I'm at a loss. The fatigue interferes with my weight loss aspirations, my work, and my daily life. Any thoughts?